Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Pelvic Inflammatory Disease Treatment
Pelvic inflammatory disease treatment aims to reduce the inflammatory process thereby arresting the growth of the organisms causing the disease. Since 60-75% of PID are caused by Sexually transmitted diseases, treatment consists of pharmacological therapy (antibiotics) to eradicate the causative organisms along with supportive therapy for the management of other symptoms. Surgical treatment may be required in case of extensive damage.
What is Pelvic inflammatory disease ?
Pelvic inflammatory disease (PID) is the inflammation of the upper genital tract involving the fallopian tubes as well as the ovaries. The inflammation is often bilateral because most of the PID is caused by the ascending or blood borne infection and the close anatomic association of the ovaries with the fallopian tubes favours the bilateral involvement, though one tube may be more affected than the other. The Pelvic inflammatory disease treatment aims to reduce this inflammation and prevent further damage to the organs.
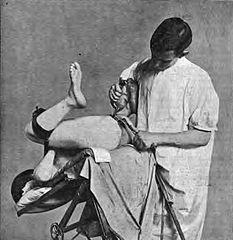
Pelvic exam - Medical Record 1896
Pelvic inflammatory disease causes
- The most common cause of PID is sexually transmitted diseases (STD)
- Most common being gonococcal and chlamydial infections
- 60-75% of PID is caused by STD, of which gonorrhoea accounts for about 30% in the developed countries
- Gonoccoci and Chlamydia travel up the genital tract along the mucous membrane to reach the fallopian salpingo-oophoritis
- Other organisms directly ascend along the lining of the genital tract
- Other organisms that cause PID include mycoplasma, tubercular bacillus, viruses and E. coli. Both aerobes and anaerobes are implicated in PID
Pelvic inflammatory disease Pathology
Acute Salpingitis
- The fallopian tube is swollen, edematous and hyperaemic with visible dilated vessels on the peritoneal surfaces.
- The sure sign of salpingitis (inflammation of the fallopian tube) is the discharge of seropurulent fluid from the fimbrial end of the tube.
- The inflammatory exudate is discharged into the lumen of the tube leading to adhesions and tubal blockage or narrowing of the lumen which may be the cause of ectopic pregnancy or infertility.
- Pelvic abscess may be formed due to pus collection in the pelvic cavity.
- The ovaries are involved and a tubo ovarian abscess or mass may result.
- In rare cases the infection may spread upwards to cause generalized peritonitis, paralytic ileus and even sub diaphragmatic and perinephric abscess.
- In PID following postabortal and puerperal infection, the infection spreads through the cervix via lymphatics to the cellular tissue causing cellulitis. The fallopian tube is affected from outside and the mucous membrane last of all.
- Pelvic inflammatory disease treatment in the acute stage helps limit the infection and prevent long term damage to the fallopian tube and ovaries leading to adhesions formation, infertility etc. In the early stage pelvic inflammatory disease treatment may only require administration of the antibiotics but in the later stage surgical drainage of the abscess and adhesions breakdown may be needed.
Pelvic inflammatory disease symptoms and signs
- The most common symptom of acute PID is lower pelvic pain. Pain is bilateral and restricted to lower abdomen.
- Pain spreads upwards if general peritonitis ensues.
- Pain is severe in acute stage and is followed by a high temperature. Vomiting may also follow.
- Discharge from the vagina and dysuria also occur.
- Menstrual irregularity if any, is due to preceding endometritis in case of ascending infection or to the antecedent abortion or delivery.
- The patient may develop uterine bleeding at a time when menstruation is not expected and the bleeding is often profuse and prolonged.
- In case of pelvic abscess, the patient develops severe diarrhoea due to rectal irritation.
Investigations in Pelvic inflammatory disease
- Haemoglobin, leucocyte count and ESR.
- Cervical and high vaginal swab culture for both aerobic and anaerobic organisms.
- Blood culture if bacteraemia sets in. C reactive protein distinguishes between infective and non infective mass.
- Ultrasound: Tubo-ovarian abscess appears on the ultrasound.
- Computed tomography shows a spherical or tubular structure with a low attenuation center.
Pelvic inflammatory disease treatment in Acute stage:
- Pelvic inflammatory disease treatment in the acute stage consists of removal of the causative organisms by proper administration of the antibiotics.
- Mild cases are treated at home with antibiotics.
- Moderate and severe cases of Pelvic inflammatory diseases may need hospitalization.
Hospital management consists of:
- Rest
- Intravenous fluids in the presence of dehydration or vomiting and correction of electrolytic imbalance.
- Antibiotics are mandatory to be instituted at the earliest for the pelvic inflammatory disease treatment even before the diagnosis is made. Initially, intravenous route is resorted to, but when the infection settles down, oral therapy may be started.
- Antibiotics like tetracycline, erythromycin, doxycycline, clindamycin are effective against both aerobic and anaerobic bacteria. Newer antibiotics include cefoxitin, cefotetan, doxycycline etc may be used for the pelvic inflammatory disease treatment.
Surgical treatment may be needed in the following conditions:
- Drainage of a pelvic abscess.
- Dilatation and evacuation of septic products of conception or for haemorrhage in postabortal sepsis.
- Acute spreading peritonitis and intestinal obstruction.
Physiotherapy management in the acute pelvic inflammatory disease
Physiotherapy aims to decrease the pain and inflammation along with the pharmacological therapy. In mild and moderate cases of Pelvic inflammatory disease where the patient does not need hospitalization, pain relieving modality like short wave diathermy can be given.
Short wave diathermy is a deep heating modality, produces heat in both deep and superficial tissues. In the acute stage very mild or pulsed short wave diathermy is used to promote healing and reduce pain.
For the Pelvic inflammatory disease treatment short wave diathermy can be given for 5-10 minutes for a period of three days a week using the cross- fire method of diathermy. Cross-fire method involves moving the electrodes to a position at right angles to their previous position half way through the treatment. Half the Pelvic inflammatory disease treatment is given antero-posteriorly through the pelvis with the patients in the lying position and second half in the side lying with the legs curled up or in sitting position and the electrodes placed over the pelvic outlets and the lumbo-sacral area of the spine.
Pelvic inflammatory disease treatment in Chronic stage:
Physiotherapy management of the pelvic inflammatory disease in the chronic stage aims at:-
- Relieving pain.
- Promote healing around the area.
- Treat existing musculoskeletal dysfunction or prevent further musculoskeletal dysfunction.
- Increase function.
Pelvic inflammatory disease treatment modalities consist of:-
- Short wave diathermy: it is widely known that short wave diathermy can be used to reduce pain and swelling, accelerate the inflammation process and promote healing in tissues with chronic inflammation. It leads to increased circulation around the area by vasodilatation leading to better healing. It also increases the metabolic activity of the area leading to more nutrients, more cellular activity and healing and increasing collagen extensibility. It helps in the repair of pelvic microcirculation, thus enabling lysis of scar tissues, relaxation of contracted muscles in the pelvis and pelvic floor.
- For the pelvic inflammatory disease treatment in the chronic stage short wave diathermy is given for 15-30 minutes, two times a day for thrice a week using the cross-fire method of treatment.
- Electrical stimulation in the form of Transcutaneous electrical nerve stimulation (TENS) to the low back for the symptomatic removal of low back pain can be given. TENS works at both spinal cord level and higher brain centres to inhibit the transmission of nocioceptors thus relieving the perception of pain.
- Moist hot pack can be given the low back to relieve pain in the lower back.
- The pelvic floor muscles in women in the chronic PID may be in the hypertonic state due to pain, delayed healing, scar tissue adhesions or generalized spasm throughout the pelvic floor tissues. Pelvic floor rehabilitation is indicated in the pelvic inflammatory disease treatment in such patients.
- Teaching control and relaxation of the pelvic floor musculature is important in these patients. Biofeedback including surface EMG can be used to induce relaxation in these muscles.
- For strengthening the pelvic floor musculature instruct the patient to tighten the pelvic floor as if attempting to stop the urine flow. Hold for 3-5 seconds and relax. Repeat 10 times per session. These exercises are done with empty bladder.
- Elevator exercises: instruct the woman to visually imagine riding in an elevator. As the elevator goes from one floor to the other, contract the muscles a little more. Relax the muscles gradually, as if the elevator were descending one floor at a time.
- For treating a woman with hyper tonus, increase the rest time between the pelvic floor contractions and sets. Emphasis on relaxation is equally important for strength training in these clients. Use of surface EMG for feedback is invaluable for enhancing awareness of holding patterns and resting tone.
- Instruct the woman to contract the pelvic floor as in the strengthening exercises then allow total voluntary release and relaxation of the pelvic floor muscles. This activity can be coordinated with breathing. Instruct the woman to concentrate on a slow deep breath and allow the pelvic floor to completely relax.
Surgical treatment
Read more articles about PID on Mayoclinic
It may be indicated in the chronic pelvic inflammatory disease where the extent of damage is more. Tubal damage may require tuboplasty. Laproscopic breaking of adhesions is indicated if the tubal blockage is due to external adhesions. On the whole surgery depends on the age and parity of the patient, the symptoms and pelvic pathology. For prevention against Pelvic inflammatory disease, delivery must be conducted in the hospitals, contraceptive devices like barrier methods must be used to prevent sexually transmitted diseases and the young women should be educated regarding the risk of STDs and its prevention.
Return from Pelvic Inflammatory Disease Treatment to Home Page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |

