Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
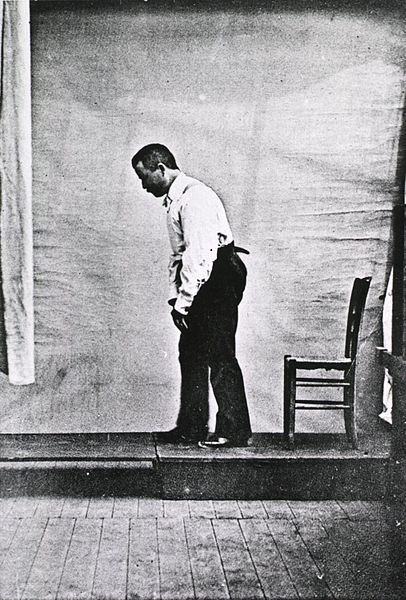
Parkinsons Disease Physical Therapy
Parkinsons Disease Physical Therapy, emphasizing gait retraining and motor control relearning, may help overcome postural instability. The individual can be trained to focus on foot positioning to provide a more stable base for posture and gait. Other helpful techniques include teaching the individual to turn around in a wide arc, rather that pivoting, in order to avoid the risk for loss of balance and postural stability, thus decreasing the risk for falls. Instructing the individual to consciously take longer steps with the help of verbal and visual (object) cues may help overcome the effects of freezing and festination. With the help of a neurologic music therapist, the physical therapist can provide parkinsons disease physical therapy exercises in a rhythmic fashion, that is, movements coupled with musical or drum-beating rhythm. Other specific exercises should include aerobic conditioning to improve endurance, strengthening of back extensor and abdominal muscles in order to promote a more upright posture, and stretching of trunk flexor muscles.
Impairments Resulting from Parkinson's Disease
Motor
Gait
Movement initiation and execution
Bradykinesia
Tremor
Rigidity
Sensory/pain
Autonomic dysfunction
Orthostatic hypotension
Constipation
Cognitive
Behavioral and affective
Depression
Anxiety
Psychotic features, such as hallucination
Gastrointestinal
Swallowing and nutrition
Constipation
Bladder dysfunction
Sexual dysfunction
Therapeutic Plan for Patients with Parkinson's Disease
Medical and Nursing
- Firm bed to decrease contractures and improve bed mobility
- Gradual changing of positions, elastic stockings, abdominal binder, sodium tablets, and possibly pseudoephedrine, midodrine, and/or fludrocortisone for orthostasis
- Regular meals with proper diet (low protein); nutritional consultation
- Measure vital capacity and enforce incentive spirometry to prevent atelectasis and pneumonia
- Bowel program for gastrointestinal hypomobility (stool softeners, bulk-forming agents, cisapride, and suppositories may be required)
- Bladder evaluation and urodynamics; anticholinergics (e.g., oxybutynin chloride [Ditropan]) for hyperreflexic bladder
- Artificial tears for lack of blinking
- Sexual dysfunction evaluation
- Anticholinergic medications before mealtime to help facilitate oral and pharyngeal movements
Parkinsons Disease Physical Therapy
- Relaxation techniques to decrease rigidity
- Slow rhythmic rotational movements
- Gentle range-of-motion and stretching exercises to prevent contractures, quadriceps and hip extensor
- isometric exercises
- Neck and trunk rotation exercises
- Back extension exercises and pelvic tilt
- Proper sitting and postural control (static and dynamic); emphasize whole body movements
- Breathing exercises stressing both the inspiratory and expiratory phase
- Functional mobility training, including bed mobility, transfer training, and learning to rise out of a chair by rocking; may require a chair lift
- Stationary bicycle to help train reciprocal movements
- Training in rhythmic pattern to music or with auditory cues such as clapping may help in alternating movements. Standing or balancing in parallel bars (static and dynamic) with weight shifting, ball throwing
- Slowly progressive ambulation training (large steps using blocks to have patients lift legs, teaching proper heel-to-toe gait patterns, feet 12-15 inches apart, arm swing; use inverted walking stick, colored squares, or stripes as visual aids)
- Use of assistive devices (may need a weighted walker)
- Aerobic conditioning (swimming, walking, cycling)
- Frequent rest periods
- Family training and home exercise program
Occupational Therapy
- Range-of-motion activities of upper extremity with stretching
- Fine motor coordination and training, hand dexterity training using colored pegs or beads
- Hand cycling to help train reciprocal movements
- Rocking chair to help with mobilization
- Transfer training
- Safety skills
- Adaptive equipment evaluation, including Velcro closures, raised toilet, grab bars, eating utensils with built-up handles, and key holders
- Family training and home exercise program
Speech
- Deep breathing and diaphragmatic breathing exercises
- Articulatory speech training for dysarthria
- Facial, oral, and lingual muscle exercises
- Swallowing evaluation, including a modified barium swallow as needed
- Teaching compensatory strategies for safer swallowing
Psychology
- Psychological support for patient, family, and caregivers
- Cognitive assessment
Pharmacotherapy of Parkinson's Disease Treatment
Levodopa: Levodopa activates D1 and D2 dopamine receptors in the brain. Carbidopa is a peripheral dopa-decarboxylase inhibitor. It increases therapeutic potency and decreases gastrointestinal side effects of levodopa
Dopamine agonists: Stimulate dopamine receptors
Bromocriptine
Pergolide
Cabergoline
Pramipexole
Ropinirole
Amantadine: Promotes synthesis and prevents reuptake of dopamine; increases dopamine release; stimulates dopamine receptors
Anticholinergics: Restore imbalance between dopaminergic and cholinergic neurotransmitters
COMT inhibitors:
Entacapone
Tolcapone
Selegiline hydrochloride (Deprenyl or Eldepryl)
Ablative and Stimulation Procedures for Parkinson's Disease
- Ablative procedures
- Thalamotomy
- Pallidotomy
- Subthalamotomy
- Deep brain stimulation procedures (DBS)
- Thalamus (Vim nucleus)
- Globus pallidus pars interna (Gpi)
- Subthalamic nucleus (STN)
- Restorative procedures
- Fetal cell transplantation
- Stem cell transplantation
Return from parkinsons disease physical therapy to Home Page
Return from parkinsons disease physical therapy to Neuro Rehab
